Macmillan Cancer Decision Support Tool (CDS) - FAQ's
What is the Macmillan Cancer Decision Support Tool Project?
The Macmillan Cancer Decision Support Tool project is part of the wider Prevention and Diagnosis programme of work by Macmillan Cancer Support. The tool displays the risk of a patient having an undiagnosed site-specific cancer, and alerts the GP during consultations when a patient has a risk of 2% or higher.
What is the Background to the Macmillan Cancer Decision Support Tool?
The Macmillan Cancer Decision Support Tool aids GPs in their clinical decision making and assists in deciding whether to refer or request further diagnostic investigation in patients where they believe there is a risk of cancer.
The Macmillan Cancer Decision Support Tool is based on the Risk Assessment Tool (RAT), developed by Professor Willie Hamilton and is currently available for the five types of cancer below:
- Colorectal
- Lung
- Gastro-oesophageal
- Pancreatic
- Ovarian
The tool displays the risk of a patient having a specific type of cancer, founded on analysis of historic population cohorts in addition to a range of factors including symptoms, medical history and demographic data.
How does the Macmillan Cancer Decision Support Tool work with Vision 3?
There are three modules to the Macmillan Cancer Decision Support Tool:
- Alerts
- Risk Assessment Template
- Risk Assessment Reports
Alerts
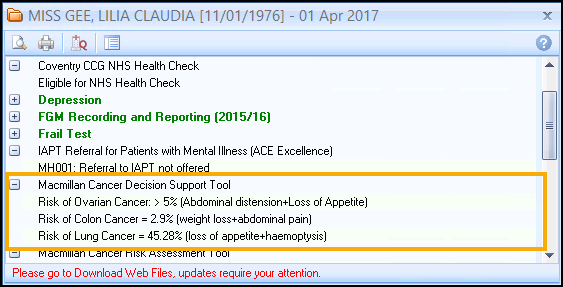
The Macmillan Cancer Decision Support Tool assesses a patient's risk score by reviewing the patient's demographic information, relevant tests and coded symptomatic information from the previous 12 months. The score is calculated and if the following criteria are met the Alert screen displays the score and the reasoning behind the value:
- A risk score of over 2% calculated for any of the 4 tumour sites included in the tool displays on the Alert screen.
- If there is a risk of over 2% for more than one tumour site then all relevant values display on the Alert screen.
Risk Assessment Template
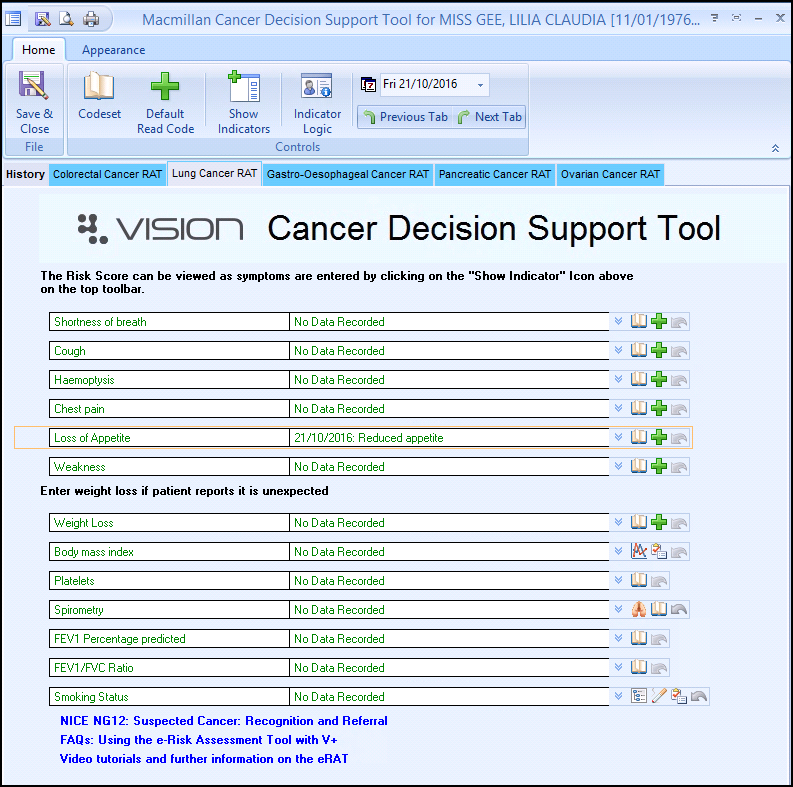
The Macmillan Cancer Decision Support Tool template allows you to record additional information during a consultation. It is an easy to use tool which allows the GP to calculate a risk score during a live consultation by selecting signs and symptoms reported by the patient. The tool only uses data from the last 12 months and calculates risk scores based on ranges built into the RAT algorithm.
Risk Assessment Reports
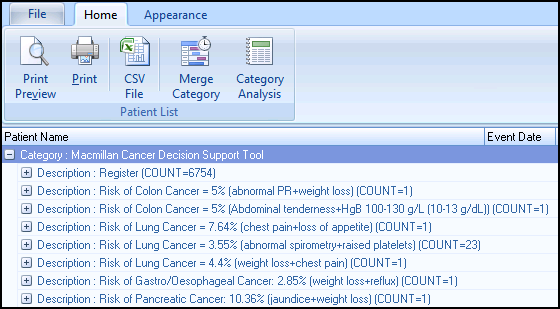
The Macmillan Cancer Decision Support Tool Practice Reports enable you to carefully monitor patients at risk of developing cancer, take appropriate actions for the patient and invite the patient for review. They display in categories making it easy to identify patients over 2% risk of developing cancer. You can quickly sort and review the patient's record from within Practice Reports or invite the patient to attend surgery.
What level of coding is required for the tool to work effectively?
It is important to note that the efficacy of the CDS tool is determined by the level of read-coded information present within each patient file. The CDS tool will be less effective in situations where limited coding of symptoms, investigations or diagnosis is carried out as the tool works by pulling this data together. In order to increase the efficacy of the CDS tool, we would recommend using the symptom checker function to calculate a risk score, before then using this same function to efficiently code selected symptoms back to the patient file. The symptom checker function therefore not only allows you to calculate live risk scores, but additionally it provides an opportunity for swift read-coding. These actions could support practices to improve their coding, safety-netting and efficacy of the CDS tool.
Do all members of the Practice need to have the tool installed?
The tool is available to all Practice staff using Vision+, and can be accessed when and if required. Any new versions of the CDS tool are made available for you to update. You are made aware that there is a new version to download within the Alert screen in Consultation Manager and within Download Web Files. You only need to download each update once which changes the template and reports for everyone in the practice.
Won't I find the prompts intrusive?
Feedback from the pilot suggested that there is a balance to be struck determining the threshold at which prompts display, and whether certain cases should be excluded from the Alert screen. Currently the alert flags patients that have a minimum of 2% risk of any of the tumour sites included in the tool.
Macmillan Cancer Support have also considered the 2015 update for the NICE recommendations on suspected cancer referral.
Will the CDS Tool run in real time in Vision+?
Any information entered during the consultation will update the patient's record and change the score automatically.
How should the CDS Tool be used?
The tool can be used as a reminder to GPs to consider the likelihood of an individual patient having specific types of cancer. It is there to support GPs in considering whether further investigations or referral would be appropriate. It is an aid to clinical decision making.
What do the risk values in the CDS Tool mean?
The risk values in the tool are the proportion of those people within the original study population, with the listed characteristics and/or symptoms, who have that cancer type.
Will using the CDS Tool raise patient anxiety of the probability of having Cancer?
The tool is designed only as an aid for GPs who will exercise their own judgement about how the tool is used in a consultation setting. Some GPs reported that a discussion about the level of risk can be useful as part of the consultation with patients.
Will the Reports include specific high risk population groups?
The reports are structured into groups which enable you to quickly identify those patients with high, medium, low and very low risk values (as calculated by the tool).
What national discussions have been held with Secondary Care regarding the potential for increased levels of referral and diagnostic activity?
It is hard to tell what impact the CDS Tool will have on the levels of referral and diagnostic activity, and is one of the areas Macmillan Cancer Support seek to measure as part of the project.
Their focus on the pilot in 2013 was to see whether an electronic assessment tool was useful for GPs in supporting their decision-making around investigation and referral. Whist they are keen to measure referral impact going forward, this was not a focus on the initial pilot evaluation. They are currently exploring options for further evaluation, and will be linking with colleagues in secondary care once they have agreed the plan and scope for evaluation.
How do these tools relate to NICE (NG12) or the Scottish Referral Guidelines for suspected cancer?
It is important to take into account that the calculation of Positive Predictive Value (PPV) risk scores by the CDS tool differs slightly to that of the NG12 guidance, as this tool is not an electronic translation of the guidance. For this reason, the risk scores from the CDS tool are not directly comparable to the risk scores discussed in the NG12 guidance. In this way, although the CDS tool and NG12 guidance both discuss PPV risk scores, the evidence which drives the risk score differs, meaning that a 3% NICE score does not directly correlate to a 3% CDS risk score.
The CDS tool does not incorporate NICE or the Scottish Referral Guidelines for suspected cancer in to the risk scores (although NG12 is based on similar evidence to that of the CDS tool) so it is not prescriptive to any guideline. Instead the tool is intended to complement all existing cancer guidelines by focusing not only on high risk patients but also those at low risk. In this way, the CDS tool can be used alongside all existing guidelines. If you would like to find out more please visit the Macmillan CDS webpage to view our CDS FAQ videos.
For more guidance regarding the Rapid Referral guidelines or Scottish Referral Guidelines for suspected cancer please visit: https://be.macmillan.org.uk/be/s-574-audio-pdf-and-ebook-downloads.aspx.
What evidence already exists for the use of the CDS Tool in Primary Care?
This work builds on previous pilots of Cancer Risk Assessment Tools, such as NCAT-led desk based lung and colorectal tool, and Macmillan's IT based lung and colorectal tool. The project is accompanied by a comprehensive evaluation, which can be downloaded from the Macmillan website.
Why does the CDS tool concentrate on these tumour sites?
The decision to primarily focus on these tumour sites was taken following recommendations from Macmillan's GP Adviser team and Clinical Reference Group, as the sites which would most benefit from early diagnosis and are challenging for GPs to deal with in terms of symptomatic presentation. They are also (mostly) not a current focus for established NHS screening programmes, and offer the greatest chance of earlier diagnosis for the largest number of patients.
What are the medico-legal implications of using this tool? Is this percentage risk score entered in the patient record?
This tool is intended as an aid to clinical decision-making, to reinforce and inform clinical opinion. GPs are not compelled to act on the basis of the scores displayed, but can consider if the score is useful in deciding a course of action for a patient. All the information driving the risk calculations is already present in the patient’s notes. Risk scores calculated by the tool are not entered into the patient record at any point; the only amendment that can be made to records is the inclusion of symptoms entered through the Template, added as the relevant/preferred clinical term for that symptom. Previous pilots of both desk based and IT based RATs have not led to medico-legal issues; additionally there have been no medico-legal issues in the development, piloting and roll out of the Risk Assessment Tool.
What proof is there of the tools' efficacy?
The tool is built using algorithms from RATs, which has a weight of evidence behind it. Peer-reviewed articles on RATs have appeared in publications including the British Medical Journal and the British Journal of Cancer. Evaluation of the 2013 pilot highlighted that of patients who were referred or intended for investigation, GPs reported that in around 20% of these cases they would have taken no action without the software. The tool was welcomed by the majority of participants because it raised awareness of cancer symptoms, reminding and alerting GPs to ‘think cancer’. The tool was useful in practices where a patient may not see the same GP on each visit. In 2014, Macmillan also won a HSJ award within the category of 'Value and Improvement in Information Technology' in recognition of our work on the Macmillan pilot. This award was followed up in 2015 by the Patient Safety Award for 'Cancer Care' and a poster win at the annual RCGP Awards in the 'Innovation' category.
At what percentage risk level will prompts display?
One of the main things Macmillan gained from the pilot is the importance of setting prompts at the right level to be effective for clinicians to use. Too low, and an element of ‘prompt fatigue’ can creep in, too high and the aim of a tool designed to identify patients at ‘low risk but not no risk’ becomes compromised. GPs and Macmillan GP Advisors, have agreed that risks of 2% and over should generate a prompt.
Does the tool link to other patient management systems? (Choose and Book, SCI Gateway)
No. To help Macmillan capture information about the clinician’s experience of using the tool, there is a section within the Template which allows you to tick relevant information about tests that they have recommended. The tool is a standalone function that does not interact with any other patient or clinical management systems that may be in place. You still need to book/schedule tests in the usual way, as per their practice protocol.
What is the threshold for smoking status?
The thresholds for smoking status are:
- Heavy smoker: 20 > cigarettes per day
- Moderate smoker: 10>19 cigarettes per day
- Light smoker: <10 cigarettes per day
Is there evidence that the tool actually increases diagnoses of cancer that would have otherwise been missed?
The aim of the pilot was to see whether the Macmillan Cancer Decision Support Tool raised awareness of cancer symptoms. From the evaluation report, Macmillan can see that this displays to have been the case in that a reported 19% of patients who were referred for further investigation would not have been if the tool had not been used. Whilst this is a relatively high figure, they are confident that these patients are being seen sooner along in the referral pathway than if the tool had not been used. Going forward, they would be keen to evaluate use of the tool and impact on referral rates and ultimately, cancer diagnoses. Their clinical reference group are currently deciding future evaluation plans with their research and evaluation team at Macmillan.
With other similar tools used in Primary Care, risk stratification leads to a specific action, for example a care plan. Why put patients on a 'risk list' using the tool without any evidence based action to take as a result of the identified risk?
The full CDS Tool is intended as an aid to clinical decision-making, to reinforce and inform clinical opinion. GPs are not compelled to act on the basis of the scores displayed, but can consider if the score is useful in deciding a course of action for a patient. All the information driving the risk calculations is already present in the patient’s notes. Risk scores calculated by the tool are not entered into the patient record at any point; the only amendment that can be made to records is the inclusion of symptoms entered through the Template, added as the relevant/preferred clinical term for that symptom. Previous pilots of both desk-based and IT based RATs have not led to medico-legal issues; additionally there have been no medico legal issues in the development, piloting and roll out of the Risk Assessment Tool.
The CDS reports that are generated are not designed to be used during a consultation. They are a reporting tool which can be used to produce a list of patients for whom a risk has been calculated. The list can be sorted by risk so that those patients for whom the risks display highest are easily identified.